What is the Plantar Fascia?
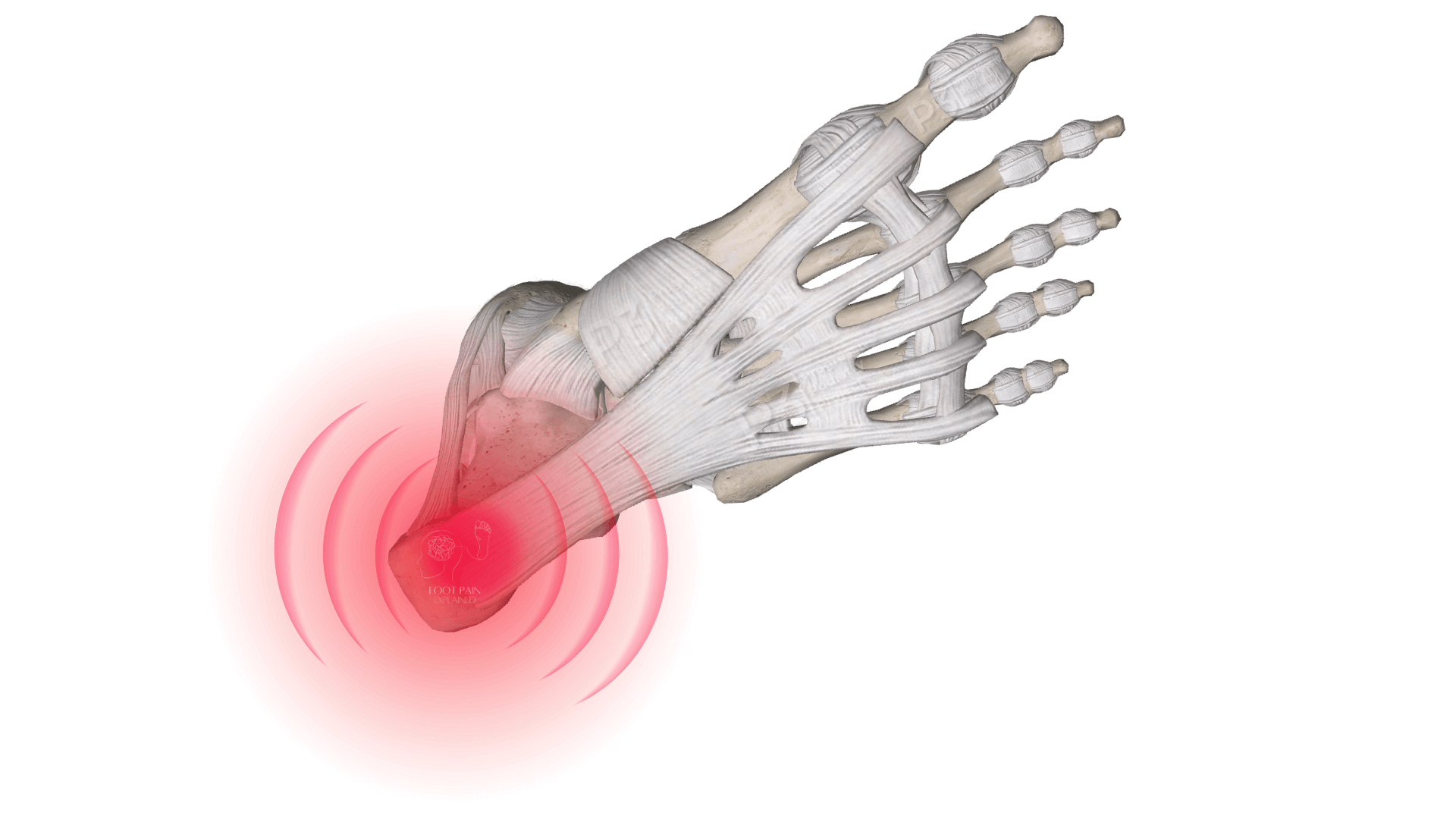
The plantar fascia is a strong, fibrous band made primarily of collagen on the bottom of the foot that supports your arch and absorbs impact during activities like walking or running. (1)
It is not a ligament.
Ligaments are built differently and function differently.
It is not a tendon.
Tendons attach muscle to bone and cause movement of joints when the muscles are contracted.
The plantar fascia is what's called an aponeurosis; a flat band of connective tissue that connects to bones, tendons and other fascia structures.

What is the Function of the Plantar Fascia?
Supports the arch of your foot:
Acts like a spring or truss that keeps your foot stable.
Absorbs impact:
Helps reduce pressure when your foot hits the ground.
Helps push-off/toe-off:
Works with your toes to give your step power during walking or running, this is known as the Windlass Mechanism.

A Closer Look at the Plantar Fascia
The plantar fascia is not just one uniform band, it has a central, medial (inner), and lateral (outer) portions (1), as well as having two distinct layers:
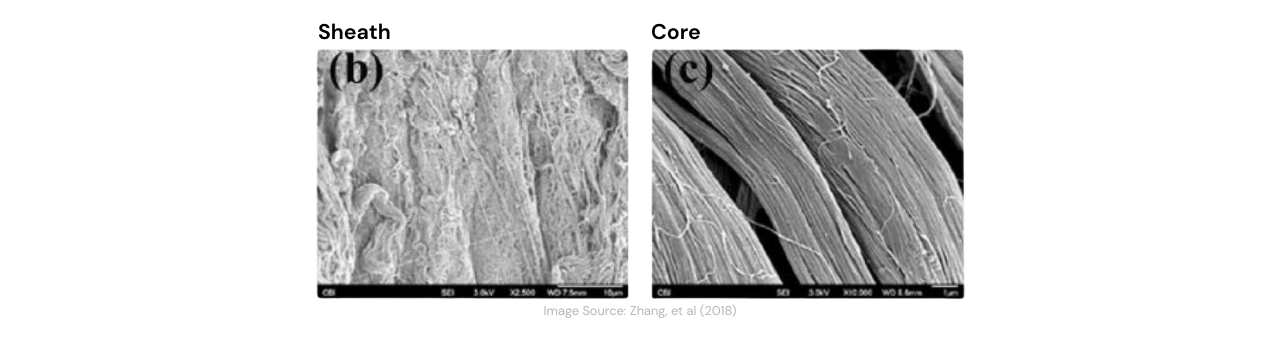
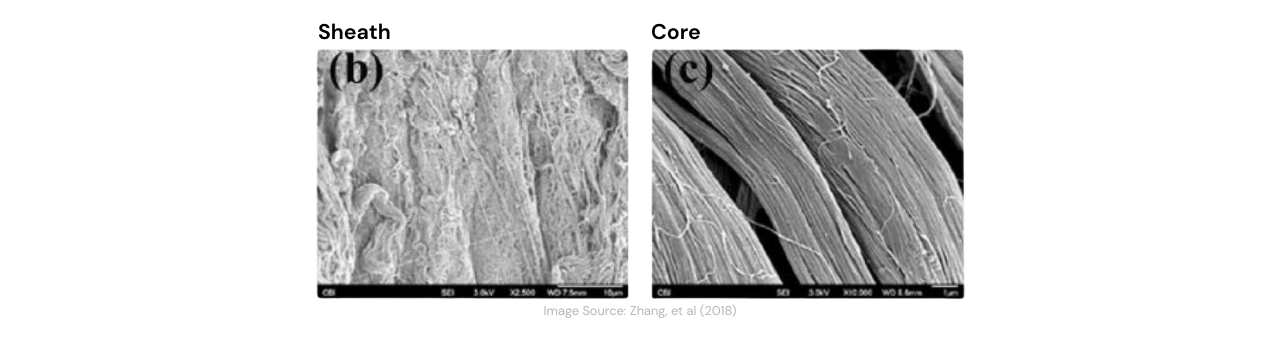
The Core:
A dense, strong centre made of tightly packed collagen fibres. This part of the plantar fascia gives it the strength to carry your body weight. (2)
The Sheath:
A softer, looser outer layer with blood vessels. This part is thought to help deliver nutrients to the structure. (2)
What is Plantar Fasciitis/Fasciosis/Fasciopathy?
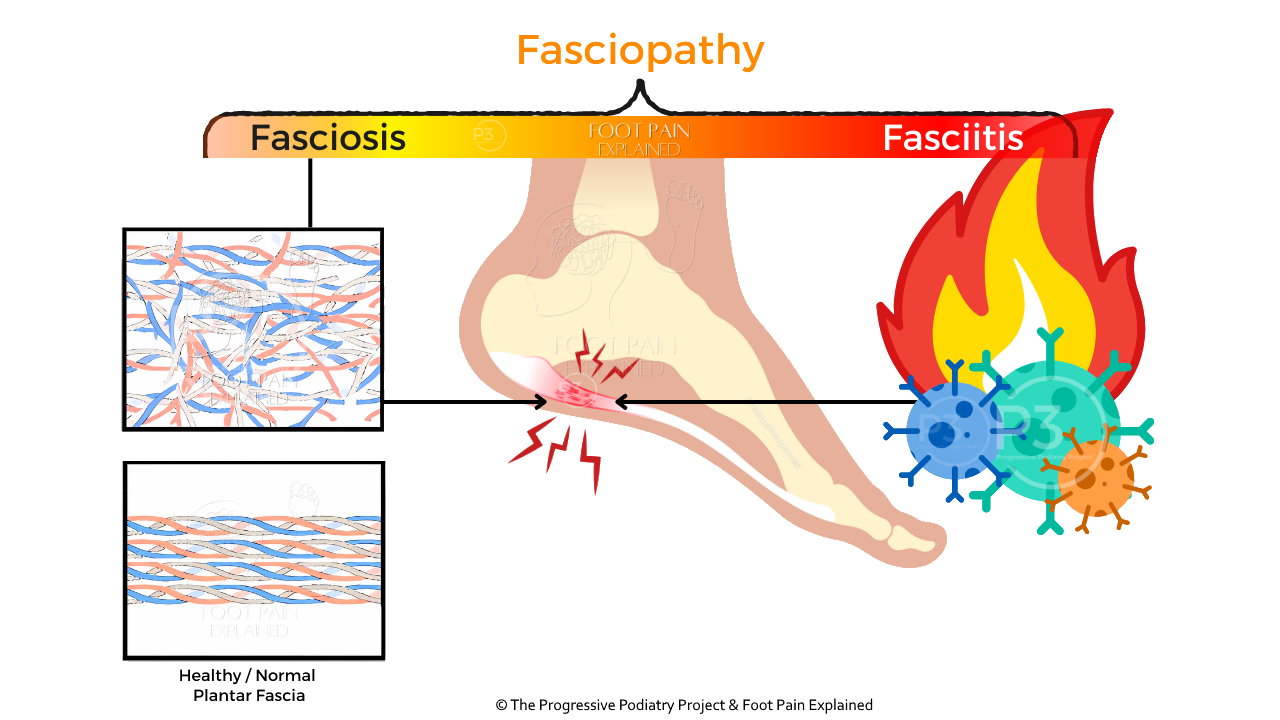
“-itis” (Plantar fasciitis): Suggests inflammation.
“-osis” (Plantar fasciosis): Refers to degeneration without inflammation.
“-opathy” (Plantar fasciopathy): Covers a spectrum of conditions, including inflammation and degeneration.
Why is it referred to as Plantar Heel Pain?
In 2017, a group of international researchers and experts on plantar fasciitis (article), due to the term fasciitis often being considered misleading.
Misleading..? Why?
'Plantar fasciitis' is too specific; fasciitis refers to inflammation of the tissue.
Remember, not everyone with heel pain will have inflammation.
Pain under the heel is common - and complex.
This is why so many people have different responses to treatments.
Learn More Here
This shift in language:
- Reflects what research now understands.
- Supports better communication.
- Can lead to more appropriate, individualised care
Who gets Plantar Heel Pain?
Plantar heel pain can present in almost any population, with some populations having higher rates than others.
Fast Facts
(Buchanan, et al, 2024) & (Rasenberg, et al, 2019)
Approximately 10% of adults will experience plantar heel pain in their lifetime.
Peak incidence of plantar heel pain in the general population is between 40 and 60 years of age.
Women tend to experience higher rates of plantar heel pain than men, in those aged between 45-64 years.
Approximately 1 in 3 patients will present with plantar heel pain in both feet.
Plantar heel pain accounts for approximately 8% of running-related injuries, with older runners having a higher incidence compared to younger runners.
Older adults & those with low activity levels (+/- high BMI) are most prone.
What are the symptoms of Plantar Heel Pain?
Common Symptoms | 'Typical' Plantar Heel Pain
Location
Pain is typically felt at the base of the heel/beginning of the arch, towards the inside part of the foot (plantar medial calcaneal area).
Pain Pattern
The most common symptom is first-step pain. Most commonly experienced first thing in the morning and after periods of rest/sitting.
Initially, the first-step pain will improve with movement ('warm-up effect').
However, as the condition progresses people may find that the warm-up effect does not occur and pain can present throughout the day.
During prolonged periods of weight-bearing/standing, especially on hard surfaces.
After periods of high loading, either immediately after, after rest, or the next day (what equates to 'high loading' will vary from person to person).
'Atypical' Plantar Heel Pain
In those with 'atypical' plantar heel pain, further investigations (e.g., diagnostic imaging and/or clinical assessments) may be required.
'Atypical' Symptoms
- Night pain.
- Acute onset/aggravation.
- Lateral (outer) heel pain.
- Posterior heel pain (back of the heel).
- Swelling.
- Neurogical symptoms (burning, tingling, numbness).
(Goff & Crawford, 2011)
What Causes Plantar Heel Pain?
Given the immensely variable presentations of plantar heel pain ('itis', 'osis', 'opathy', 'typical vs atypical' symptoms etc), no one causative mechanism has been identified.
However, the underlying cause of plantar fasciopathy is thought to be similar to tendinopathy.
With imaging & histopathological (microscopic evaluation) findings support this theory.
(Rajasekaran & Finnoff, 2015)
Repetitive stress / loads are considered to be a primary driver of pathological development
(+/- the interplay of an person's individual risk factors).
What are the Risk Factors for Plantar Heel Pain?
Despite what much of the (mis)information on the internet and social media suggests, pronation is not a large risk factor for developing plantar heel pain.
There are some populations where pronation or a 'flatter foot' (pes planus) in addition to other factors may increase a person's risk for developing the condition.
However, there are other populations where having a high-arched foot (pes cavus) may increase a person's risk.
Identified Risk Factors for Plantar Fasciopathy based on the research paper by Beeson, 2014: Plantar Fasciopathy: Revisiting the Risk Factors
Intrinsic Risk Factors (related to the body) | These are individual characteristics or physical conditions that may increase the risk of developing plantar fasciopathy:
- Limited ankle dorsiflexion (restricted upward movement of the foot) | Possibly the strongest known risk factor.
- Reduced range of movement in the calf muscles and (sometimes) hamstrings.
- High body weight or BMI | BMI > 30 kg/m² significantly increases risk.
- Changes in morphology of the plantar fat pad.
- Age-related changes | Changes to cellular structure of connective tissues.
- Foot posture and biomechanics | Both pes planus (flatter arch) and pes cavus (higher arch) feet are risk factors in certain populations.
- Gender (possibly) | Men - stiffer connective tissue in general, Women - changes in hormones around menstrual cycles, pregnancy, and menopause.
- Underlying inflammatory diseases | Autoimmune conditions (e.g., rheumatoid arthritis) may contribute in a minority of cases
Extrinsic Risk Factors (related to lifestyle or environment) | These relate to behaviours, activities, or conditions that increase mechanical load on the plantar fascia:
- Prolonged weight-bearing | Especially on hard surfaces.
- Jobs or lifestyles that involve standing/walking >80% of the day | Particularly significant in overweight individuals.
- Sudden increases in physical activity or exposure to unaccustomed activity (such as starting a new walking or running routine too quickly).
- Inappropriate footwear for the individual or activity | Not everyone needs "supportive shoes"!
- Training errors | Changes in training loads, inadequate rest/recovery etc... Sport-related overuse.

How is Plantar Heel Pain / Plantar Fasciopathy diagnosed?
A correct diagnosis can often be achieved based on symptoms and clinical assessment alone, with diagnostic imaging not being required.
What are the symptoms of Plantar Heel Pain?
Common Symptoms | 'Typical' Plantar Heel Pain
Location
Pain is typically felt at the base of the heel/beginning of the arch, towards the inside part of the foot (plantar medial calcaneal area).
Pain Pattern
The most common symptom is first-step pain. Most commonly experienced first thing in the morning and after periods of rest/sitting.
Initially, the first-step pain will improve with movement ('warm-up effect').
However, as the condition progresses people may find that the warm-up effect does not occur and pain can present throughout the day.
During prolonged periods of weight-bearing/standing, especially on hard surfaces.
After periods of high loading, either immediately after, after rest, or the next day (what equates to 'high loading' will vary from person to person).
'Atypical' Plantar Heel Pain
In those with 'atypical' plantar heel pain, further investigations (e.g., diagnostic imaging and/or clinical assessments) may be required.
'Atypical' Symptoms
- Night pain.
- Acute onset/aggravation.
- Lateral (outer) heel pain.
- Posterior heel pain (back of the heel).
- Swelling.
- Neurogical symptoms (burning, tingling, numbness).
(Goff & Crawford, 2011)